October 20,2021
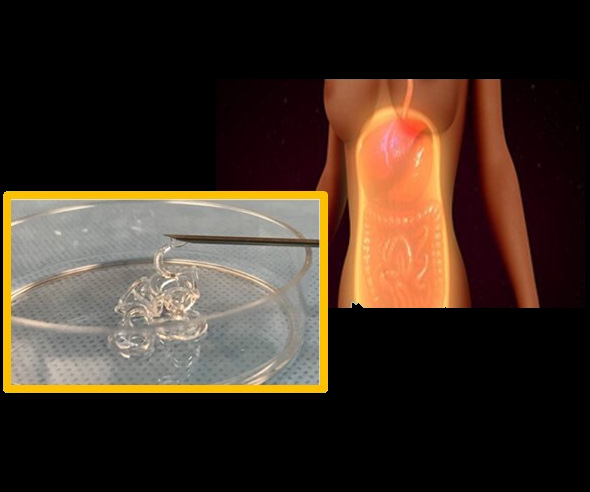
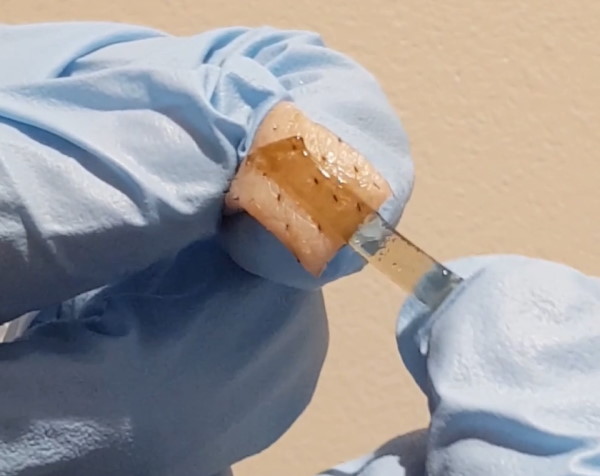
Preventing Postsurgical Adhesions using Hydrogel Barriers
(LOS ANGELES)–Following surgery within the abdominal or pelvic cavities, scar tissue often forms on the inner linings of these cavities and may adhere to the organs which are found within them. This adhesion occurs in 93% of these patients and can affect the intestines, liver, urinary bladder, gall bladder and female reproductive organs. In up to 20% of adhesion cases, serious complications can arise, including chronic abdominal or pelvic pain, fertility problems or intestinal obstruction. This not only results in increased patient suffering and mortality but adds over $1 billion in additional hospital costs in the United States alone.